Background
Personalized medicine provides a unique opportunity for patients to receive optimized treatment efficacy through individually tailored and targeted therapies. The ability to control the release of therapeutics in targeted tissues with a desired spatial distribution and at an adjustable rate is essential for personalized medicine. However, it is extremely challenging to control the release of a therapeutic drug with the desired timing, while also monitoring the real-time drug distribution in optically turbid deep tissue. This project addressed these critical issues in a controlled drug release, by developing a cross-disciplinary approach using an ultrasound technique to trigger a drug release from liposomes, in conjunction with a photoacoustic tomography technique, to quantify the dynamic profiles of drug concentrations in a tissue-mimicking 3D scaffold model.
Approach
To achieve the objective, SwRI engineered acoustic-sensitive liposomes to achieve an ultrasound-controlled delivery of therapeutic drugs. UTSA developed a photoacoustic tomography system that quantified ICG distribution in a 3D tissue model. SwRI and UTSA collaborated to detect the ultrasound-mediated drug release in a 3D tissue model using photoacoustic tomography.
Accomplishments
We have demonstrated a liposome formulation with 1) high fluorescence dye and drug diclofenac loading efficiencies, 2) high colloidal stability (-30 mV), 3) small size (100 nm) for long circulation half-life, and 4) the ability to trigger up to an 80 percent release of drug/dye payload upon exposure to one minimal treatment (5–10 minutes) of ultrasound. We also demonstrated a liposome formulation capable of dually loading a fluorescent dye and a small molecule nonsteroidal anti-inflammatory drug (NSAID), diclofenac, with a very high colloidal stability (-65 mV). The liposomes are small in size (100 nm) and ultrasound sensitive. An external ultrasound stimulus using medium frequency focused ultrasound (MFFU) at 250 kHz was used to trigger the release of 50 percent of liposomal payload after one five-minute application and greater than 90 percent payload release after four treatments (see Figure 1).
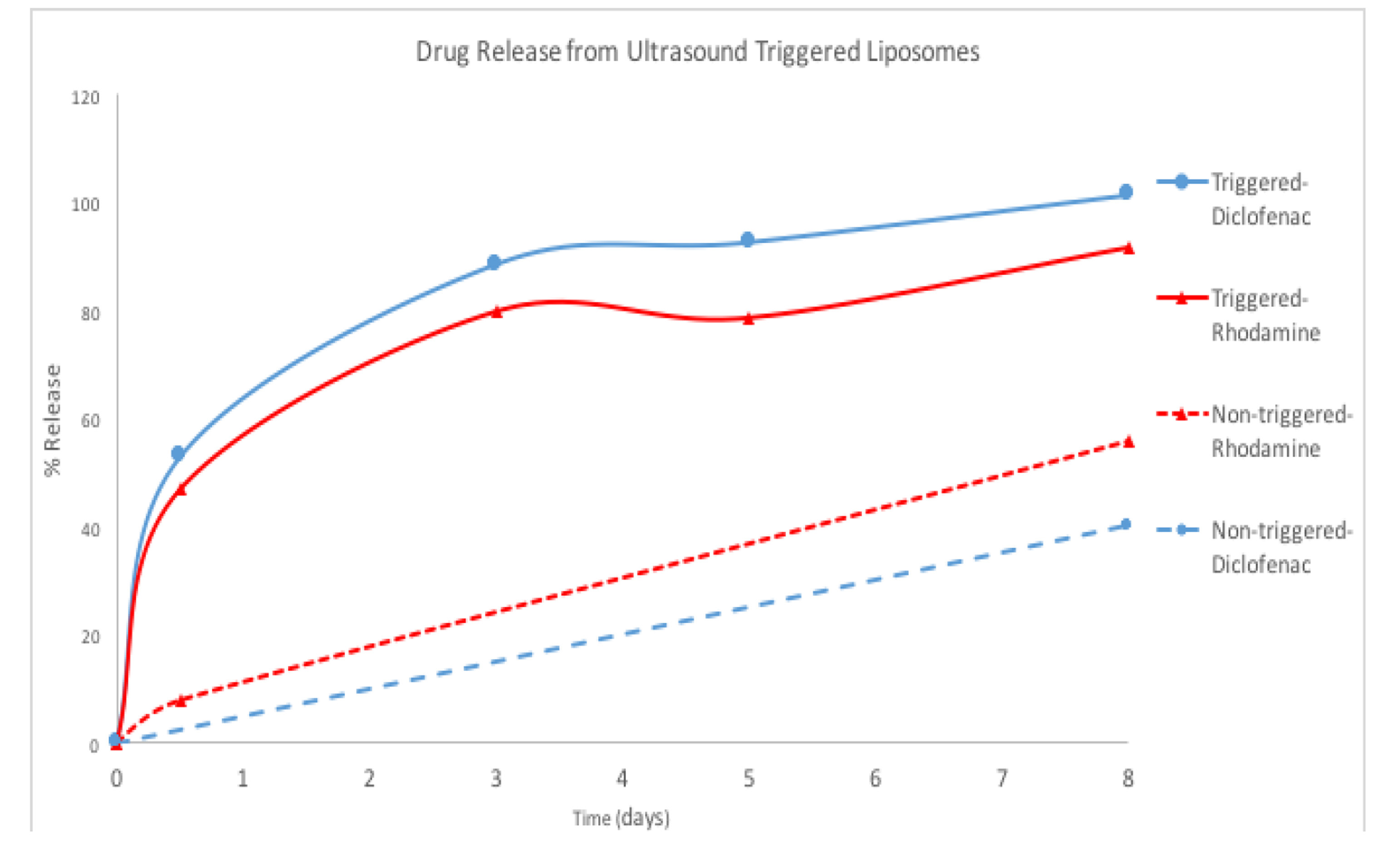
Figure 1: The top solid lines illustrate the rhodamine and diclofenac release profile from liposomes triggered by MFFU at 260 kHz. The bottom dashed lines illustrate the non-triggered control case.

